Health Insurance & The Billing Process
Meaningful Change: Clinical & Consultation Psychology contracts with a number of insurance companies in addition to accepting direct pay from clients. Although our office will review your health insurance eligibility and benefits as part of the intake process, we recommend that you verify your mental health benefits with your insurance provider so that you have a good understanding of your coverage prior to your first appointment. We are considered in-network with the following health insurance carriers.
Blue Cross Blue Shield of Michigan
Priority Health
Blue Care Network
Aetna
Blue Cross Blue Shield
Medicare Part B
Humana
We do not accept any Medicaid Plans
Insurance, Co-Payments, Deductibles & Fees
Third party payors are considered a method of reimbursement and should not be considered a substitute for client fees. As such, clients are ultimately responsible for the costs of services received which may include rejected payments by insurance providers, or services not covered by their insurance carrier that may include Co-Payments, Co-Insurance & Deductible amounts. These are due at the time of service.
For those unfamiliar with health insurance, some definitions may be helpful:
Deductible: The amount of money that the insured person must pay themselves before their insurance policy starts paying for covered expenses.
Co-Payment: A defined dollar amount that a patient pays for services. This is defined by your healthcare plan and not by our office.
Co-Insurance: A defined percentage of a given service fee that the patient is responsible for. This is defined by your healthcare plan and not by our office.
Out-of-pocket Maximum: The maximum amount that a patient has to pay within a given year before the insurance carrier covers 100% of expenses. This is typically a large amount, and is defined by your healthcare plan and not by our office.
Bills, Invoices & Receipts
In our efforts to burden clients with financial complexities as little as possible, Meaningful Change: Clinical & Consultation Psychology utilizes a minimal contact, and paperless model for billing. The practice requires that a credit, debit, or flex spending/HSA card is kept in our secure electronic record for billing purposes. When insurance claims are processed, any fees you have incurred, which may include deductible costs or co-pays, are billed to the card on file. This is also true for direct pay expenses, cancellation fees, or any administrative costs. As such you will not receive routine bills, invoices, or receipts from us. A comprehensive billing history may be found in your patient portal.
Meaningful Change: Clinical & Consultation Psychology also maintains strict standards on delinquent payments. Routine failure to make payments in a timely fashion, expired credit/debit cards, and inactive payment methods are addressed quickly with a streamlined procedure that is detailed here. Routine delays or delinquencies in payments may lead to a discontinuation of services.
Since most of our clients track their expenses online, we have found the patient portal to be a minimalistic and effective model. However, if you would like a physical invoice or receipt, please feel free to request one from our administrative staff via support@meaningfulchange.com.
Out-of-network Billing
While we typically discourage this process, patients that are motivated to see our treatment providers, but use insurance that we do not contract with, may still submit claims for reimbursement. Under these circumstances, Meaningful Change: Clinical & Consultation Psychology will bill patients our standard fees for services and then provide you with a "Superbill" that you can submit to your insurance company. The practice is willing to consider these carriers on a case-by-case basis.
Please inquire directly at support@meaningfulchange.com.
No Surprise Act
Enacted in January of 2022, the “No Surprise Act” requires that patients who pay directly for services, or those who receive services from out-of-network providers, be given a good faith estimate (GFE) for the anticipated cost of services. The law is intended to protect patients from unanticipated expenses within a treatment facility. The GFE is provided at the outset of services and whenever there are changes to a treatment plan that may affect the duration of care. If GFE documentation has not been provided to you by your treatment provider in a timely fashion, please notify them without delay, or contact our office directly. The NSA does not apply to clients utilizing insurance and seeing in-network providers. The comprehensive details about the NSA can be found here: https://www.cms.gov/nosurprises
Income-based Fees For Service
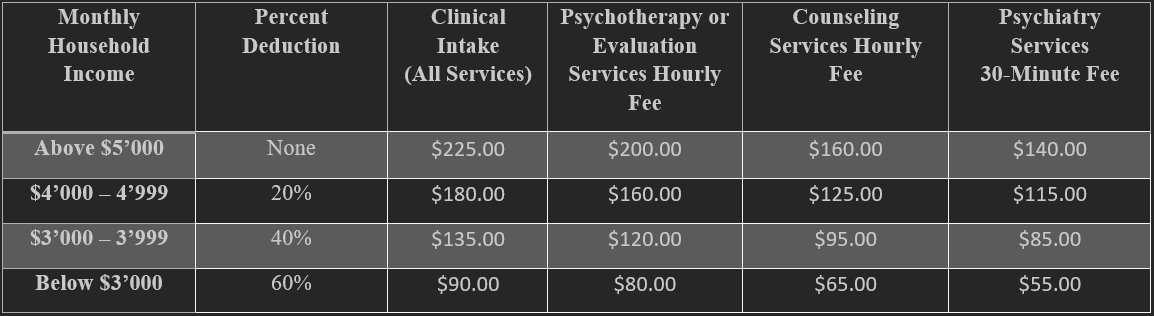
Meaningful Change: Clinical & Consultation Psychology endeavors to accommodate income-based fees for clients who are financially unable to afford services at the standard rates. These reduced rates are based on monthly household income and apply to psychotherapy, medication management, and counseling services, but not for professional consultation or evaluative services. The process is detailed below.
How to Request Income-Based Services
As fee agreements are established at the outset of treatment, interested clients may request an income-based fee during the routine intake process. Clients will be asked to declare and subsequently demonstrate their income, often in the form of two recent pay stubs, or with evidence of tax filing. Fees are established based on the table below.
*Please note that Meaningful Change can only accommodate a limited number of these clients at a time, and a request for income-based services, does not guarantee an outcome.